IBS Subtypes Explained: Why One-Size-Fits-All Advice Isn’t Enough
If you’ve been diagnosed with Irritable Bowel Syndrome (IBS), you’ve likely been given broad dietary advice or prescribed a generic medication - but the truth is, IBS is not a single condition. It has multiple subtypes, each with its own nuances and likely root causes.
Understanding your IBS subtype isn’t just helpful - it’s essential for finding the right strategy to finally get relief.
In this guide, we’ll explore:
The key differences between IBS-C, IBS-D and IBS-M
Common underlying drivers for each subtype
Personalised testing and treatment strategies that work
How to take the first step with root cause identification
What Are the Subtypes of IBS?
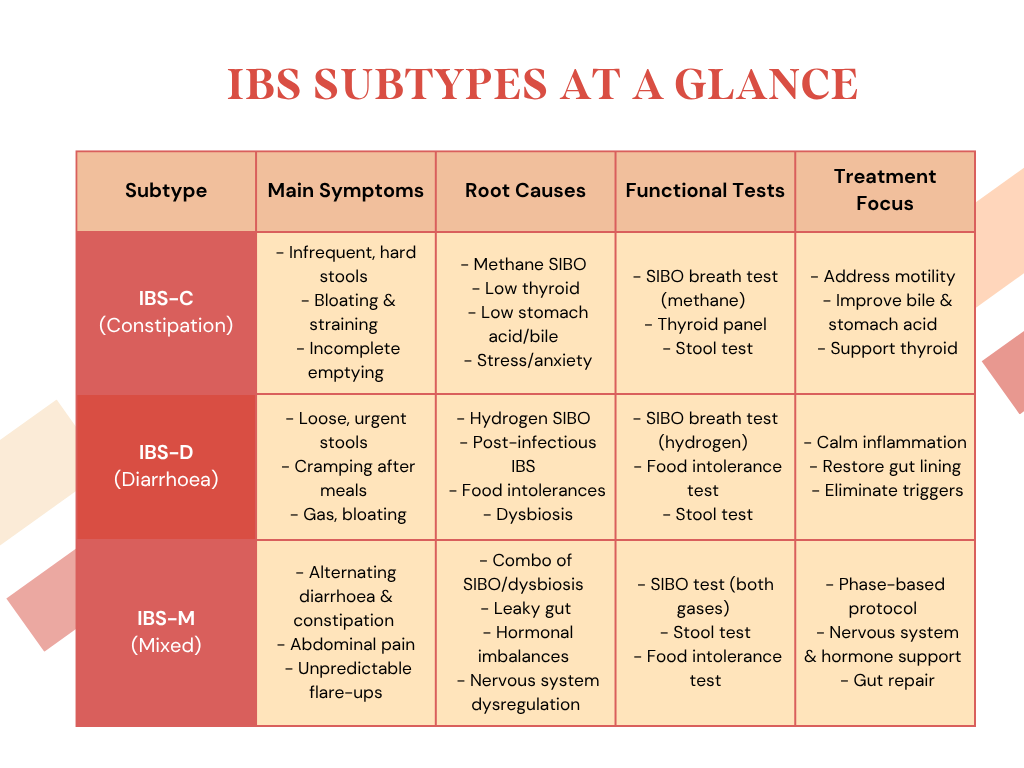
IBS is classified into three main subtypes based on your predominant bowel pattern. While the symptoms may overlap, the underlying imbalances–and the best way to treat them–can differ significantly.
1. IBS-C (Constipation-predominant IBS)
If you have fewer than three to five bowel movements per week, experience straining, and often feel like you haven’t fully emptied your bowels, you may fall into this category.
Common symptoms:
Hard or lumpy stools
Bloating and gas
Abdominal discomfort
Incomplete evacuation
Potential root causes:
Methane-dominant SIBO: Methane-producing bacteria in the small intestine slow bowel motility.
Low thyroid function: Hypothyroidism can reduce gut transit time.
Low stomach acid or sluggish bile: This can impair digestion and cause constipation further down the line.
Stress-related nervous system dysregulation
Testing to consider:
SIBO breath test (to assess methane levels)
Thyroid function panel
Comprehensive stool analysis
2. IBS-D (Diarrhoea-predominant IBS)
Frequent, loose stools, urgency, and abdominal pain are hallmarks of this subtype. It can feel like your digestion is totally out of control.
Common symptoms:
Frequent bowel movements
Urgency
Abdominal cramping
Gas or bloating
Fatigue
Potential root causes:
Hydrogen-dominant SIBO: Fast fermentation in the small intestine increases gut motility.
Post-infectious IBS: Food poisoning or travel bugs can lead to immune changes in the gut.
Food intolerances: Particularly lactose, gluten, or high FODMAP foods - however we can develop sensitivities to ANY food groups, so it’s always worth testing to find out
Dysbiosis: Imbalances in the large intestine microbiome.
Testing to consider:
SIBO breath test
Food sensitivity testing
Stool testing (for inflammation, pathogens, and microbiome balance)
3. IBS-M (Mixed-type IBS)
Do you experience both constipation and diarrhoea, sometimes in the same week - or even the same day? You may have IBS-M, the most unpredictable and frustrating subtype.
Common symptoms:
Alternating bowel habits
Bloating
Abdominal pain
Food-related flare-ups
Potential root causes:
A combination of the above, often involving stress, microbial imbalance, and digestive insufficiencies
Leaky gut: May exacerbate symptoms by increasing immune reactivity
Hormonal fluctuations (common in women with IBS-M)
Testing to consider:
Comprehensive stool analysis
SIBO testing (some cases have both hydrogen and methane overgrowth)
Food sensitivity panels
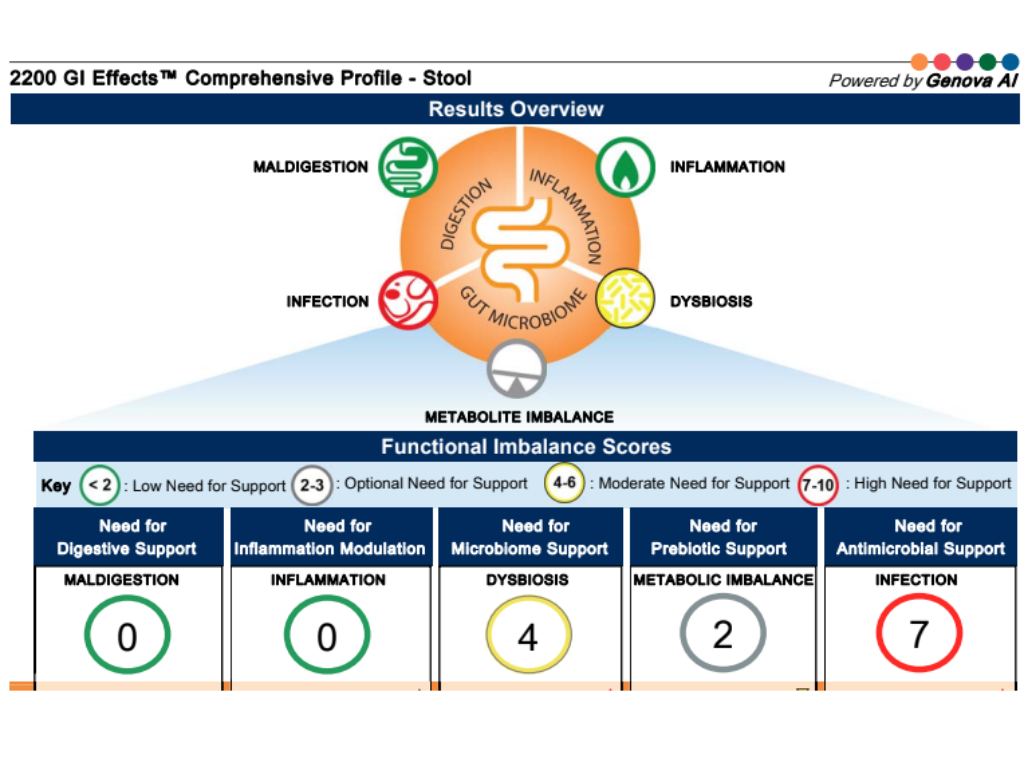
You can read more information about the functional tests mentioned above by clicking here:
Why Subtype-Specific Strategies Work
Treating IBS effectively means tailoring your approach - not just to your symptoms, but to the root causes driving them.
For example:
Someone with IBS-C due to methane SIBO will need antimicrobial protocols and motility support.
A person with IBS-D triggered by post-infectious immune dysfunction may benefit from gut-healing nutrients, probiotics, and targeted anti-inflammatories.
Someone with IBS-M might require a phased approach addressing multiple systems - including the nervous system, digestive function, and immune regulation.
This is where functional medicine and advanced testing shine. They allow us to go beyond labels and uncover the unique puzzle pieces contributing to your IBS.
Take the next step: Identify Your Root Causes
IBS is a spectrum condition. Knowing your subtype is the starting point - but finding the cause is how we map your path to long-term relief. Join the many clients I work with every day that are overcoming their IBS symptoms - often for the first time in decades!
Download my Free IBS Root Cause Quiz to begin identifying what might be driving your symptoms.
Book a Free Discovery Call to explore how one-to-one support and personalised testing can transform your gut health.
“I started working with Ellie to address some longstanding gut issues and I can honestly say I’ve never felt so confident that my digestive system is now in the best place! I’ve experienced fewer energy crashes and brain fog. I really trust Ellie, she is very knowledgeable and experienced, and can deliver great results.”
“I contacted Ellie after struggling with IBS that was seriously affecting my quality of life. From our very first conversation, Ellie’s expertise and supportive approach made a real difference. She helped me identify and manage my IBS triggers and guided me through a healing process for SIBO. I noticed improvements almost immediately after putting her expert advice into practice.
A few months on, I’m now just about symptom-free—something I never thought I’d be able to say. Ellie’s bespoke, detailed protocols have been invaluable in keeping me on track. I truly can’t thank or recommend her enough.”